< Cancer screening
Breast/Chest screening
On this page:
Breast/chest screening is a type of health check that assesses if you are at risk of developing breast cancer. It’s also known as a mammogram. We use ‘chest’ here because, for some people who were presumed female at birth (PFAB) and who have breast tissue, this term might better reflect the relationship some of us have with our bodies.
To develop this page, we worked with the ACON team responsible for Our United Front and who lead ACON’s work addressing cancer prevention in LGBTQ+ communities.
Anyone with breast tissue, whether cis or trans, regardless of your gender, can develop breast cancer. This can include those who’ve had top surgery, or had breast implants.
ACON’s Our United Front campaign seeks to increase LGBTQ community awareness about the importance of regular screening.
It is recommended that you screen once every two years from the age of 50, if you currently have, or have ever had breast tissue.
Your doctor may recommend screening more frequently depending on your family history, or a previous breast/chest tissue cancer diagnosis.
Specific recommendations for trans people between the ages of 50 and 74 years are:
Been on feminising hormones for 5+ years? Screen every two years
Haven’t had top surgery? Screen every two years
Have had top surgery and have some remaining tissue? You may need to screen every two years so chat with your doctor
If you have symptoms, such as a lump, or a thickening of discharge from the nipple, it’s important to see your doctor as soon as possible. Screening is not available for people with symptoms.
Mammograms
A mammogram is a low-dose x-ray of breast/chest tissue. The x-ray pictures can detect the presence of breast cancers as small as a grain of rice, before they can be seen or felt.
The appointment takes about 20 minutes in total, and is free at BreastScreen NSW for all women (trans and cis), who are 40+. Men and non-binary people can visit your doctor.
Self examination
Self examination or a ‘self check’ is not a replacement for mammograms, but can be done at any age where breast or chest tissue is present.
The goal of a self examination is to recognise any changes in the texture of the tissue, or to feel for any small lumps, any discharge, crusting, ulcer, redness, or inversion of the nipple. If you have any pain in breast/chest or armpit that doesn't go away, or a change in breast/chest shape, visit your doctor.
If anything else has changed, or if you’re not sure but are worried, visit your doctor and, with your consent, they can do a follow up exam and refer you on to further testing, if necessary.
It is important to remember that 8/10 lumps that appear in breast/chest tissue are not breast cancer, and instead are cysts or a similarly sized growth. Even so, it is important to go and talk to a doctor just so you know that it is benign (not harmful).
How to self screen
Even when if you’re eligible for a mammogram, you can always do a check of your own body.
Visual check: do a visual check in the mirror. Does anything look different to usual, including any noticeable lumps, redness, or swelling?
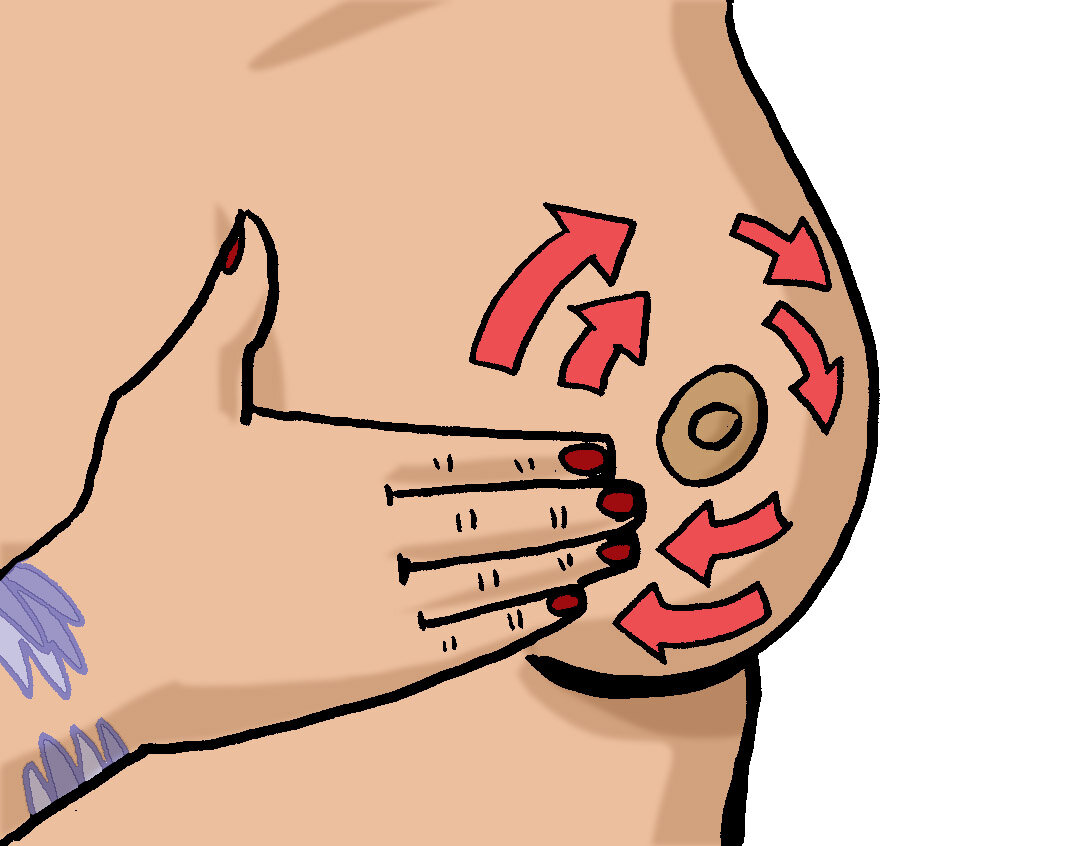
Check standing up: Raise your arm, and use your opposite hand to check the breast/chest and armpit. Work around in circles from the nipple outwards, or in and up and down motion (like mowing a lawn). This can be easier to do in the shower when things are already slippery.
Check lying down: With your arm raised, check the breast/chest and armpit like when you were standing up.
Don’t forget to check your nipples, and take note of if anything seems different or off, including new or unusual secretion.
If you find something unusual, don’t panic, and book in to see your doctor. Lumps can appear in breast or chest tissue for a range of reasons, and not all of them are dangerous or harmful. Letting your doctor know means you can be sure and look after your health.
For some trans people, interacting with our chests is distressing and might exacerbate dysphoria. Self examination may feel difficult or impossible, and that’s totally okay. We recommend having a chat with your doctor about methods and time-frames to make sure you’re looking after your health but still feeling affirmed.
Downloads
10 trans questions to ask a doctor - TransHub [ Plaintext version ]
Doctor letter: affirm name and pronouns - TransHub